The Effect of the Diet and Other Genetic Factors on a Unique β-Thalassemia Genotype IVS1.1 [G>A] / IVS2.1 [G>A] Discovered in Kirkuk City
Abstract
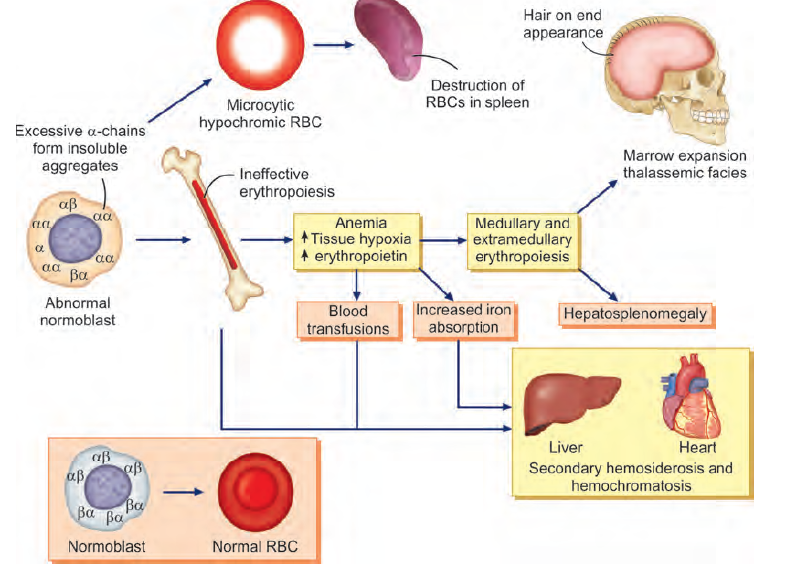
Background: Thalassemias are inherited hemoglobin disorders characterized by reduced or absent globin chain synthesis, resulting in a variety of clinical phenotypes ranging from severe chronic anemia requiring lifelong transfusion and iron chelating therapy to asymptomatic individuals.
Methods: The study was done on a family consisting of four individuals, a minor father and a minor mother (carriers), major two daughters. During sampling, one of the girls has facial deformities and a typical thalassemic face with changes on the skull (younger daughter B). The older daughter(A) has no facial deformities and has a normal skull like a healthy non-thalassemic individual.
The study aimed to detect if the two daughters have the same mutations and the reason for the differences in facial bone deformities between them.
The results were obtained by reverse hybridization using B- globin strip assay MED and pedigree analysis of the family.
Results: The two thalassemia major daughters have a unique genotype never seen before in another study IVS1.1 [G>A]/ IVS2.1 [G>A]. Each mutation inherited from the minor mother IVS2.1 [G>A] and minor father IVS1.1[G>A]. The combination of the two mutations is seen first in this family never seen before in another study. This new combination in the two intervening sequences 1,2 on the B-globin gene sequence causes a complete absence of a beta chain. That means the two daughters are thalassemia major [B0/B0].
Conclusion: The genotype IVS1.1[G>A]/IVS2.1[G>A] (B0/B0) is unique and first seen in Kirkuk city. The phenotypes between the two daughters were affected by the diet and the mutation in the MCIR gene.
References
Srichairatanakool, S., Koonyosying, P., & Fucharoen, S. (2020). Diet-Related Thalassemia Associated with Iron Overload. In (Ed.), Personalized Medicine, in Relation to Redox State, Diet and Lifestyle.
Al-Momen, H., Hussein, H. K., Al-Attar, Z., & Hussein, M. J. (2020). Green tea influence on iron overload in thalassemia intermedia patients: a randomized controlled trial. F1000Research, 9, 1136.
Fung, E. B., Xu, Y., Trachtenberg, F., Odame, I., Kwiatkowski, J. L., Neufeld, E. J., Thompson, A. A., Boudreaux, J., Quinn, C. T., Vichinsky, E. P., & Thalassemia Clinical Research Network (2012). Inadequate dietary intake in patients with thalassemia. Journal of the Academy of Nutrition and Dietetics, 112(7), 980–990. https://doi.org/10.1016/j.jand.2012.01.017
Nayak, R., and Rai, Sh. (2017).Thalassemia Syndrome. Essentials in hematology and medical pathology, (2nd ed). Pages: (58-66), New Delhi/London: Jaypee brothers medical publishers (p) 2 Ltd.
Whitley,K.S. and Kwiatkowski ,J.L.(2020). Hemoglobinopathies. InNelson’s Textbook of Pediatrics , Elsevier Inc,pages 2540-2558 .e1.
Randolph,T.R.(2020).Thalassemia.In McKenzie, Sh. B., Landis-Piwowar, K and Williams, J.L.(Eds.), Clinical Laboratory Hematology,(4th ed), by Pearson, pages 289-313.
Chapin,j. and Giardina,J.(2018).Thalassemia Syndromes. In Hoffman, R(ED.), Hematology, (7th ed), Elsevier, pages 456-570.e10.
Cappellini, M.D.(2020). The Thalassemias.IN Goldman-Cecil medicine (26th ed), Elsevier, pages 1055-1061.e2.
Rathore ,R.(2022) .Thalassemias .In Ferri’s Clincal Advisor , Elsevier, pages 1470.e9-1470 .e15 .
Lawrence, C.and Meier, E.(2021) Erythrocyte disorders. In Dietzen, D. Bennett, M. Edward Wong, E., Shannon Haymond, SH.(Eds), Biochemical and Molecular Basis of Pediatric Disease (Fifth Edition), Academic Press, Pages 529-560.
Ali, S., Mumtaz, S., Shakir, H. A., Khan, M., Tahir, H. M., Mumtaz, S., ... & Khan, M. A. (2021). Current status of beta‐thalassemia and its treatment strategies. Molecular Genetics & Genomic Medicine, 9(12), e1788.
Skordis , N. and Kyriakou, A.(2021). Bone disease. In Cappellini, M.D., Farmakis, D., Poter, J., and Taher, A. (Eds.), Guidelines for the management of transfusion dependent thalassemia (TDT), (4th ed), Thalassemia international federation, pages 180-191.
Holstein ,S.A.and Hohl ,R.J.(2021).Thalassemia. In Conn’s Current Therapy, Elsevier, pages 483-488.
Khandros, E. And Kwiatkowski,J.L.(2022).Hemoglobinopathies.In Fish, J. D., Lipton, J. M., & Lanzkowsky, P. (Eds.),Lanzkowsky's manual of pediatric hematology and oncology,(7th ed ), Elsevier, academic press, pages 161-192.
Porter, J.(2021). Iron overload: Pathophysiology, diagnosis and monitoring. In Cappellini, M.D., Farmakis, D., Poter, J., and Taher, A. (Eds.), Guidelines for the management of transfusion dependent thalassemia (TDT), (4th ed), Thalassemia international federation, pages 56-71.
Britannica, T. Editors of Encyclopaedia (2018, September 18). pedigree. Encyclopedia Britannica. https://www.britannica.com/science/pedigree-genetics
Shalaan, O., Sakr, M., Daif, A., & Elhalfawy, K. (2016). Rapid and simultaneous detection of β-thalassemia point mutations by reverse hybridization strip assay among Egyptian patients. Journal of Biochemistry, Microbiology and Biotechnology, 4(1), 11-14.
Beta-Globin StripAssay(R) MED (Ref 4-130, ViennaLab Diagnostics GmbH).
Adekile, A., Haider, M., & Kutlar, F. (2005). Mutations associated with beta thalassemia intermedia in Kuwait. Medical Principles and Practice, 14(Suppl.1), 69-72.
Kuan, J. ,Kole, R. , Nielsen, P.& Glazer, P. (2006). 89. Gene Targeting of β-Globin IVS2 Using Sequence-Specific Peptide Nucleic Acids. Molecular Therapy - MOL THER. 13. 1.
Gomes, W. R., Santos, R. A., Cominal, J. G., & Tavares, C. F. (2017). Frequencies of CD39, IVS1-1, IVS1-6 and IVS1-110 mutations in beta-thalassemia carriers and their influence on hematimetric indices. Jornal Brasileiro de Patologia e Medicina Laboratorial, 53, 362-367.
Kumar, R., Arya, V., & Agarwal, S. (2015). Profiling β Thalassemia Mutations in Consanguinity and Nonconsanguinity for Prenatal Screening and Awareness Programme. Advances in hematology, 2015, 625721.
Denic, S., Aden, B., Nagelkerke, N., & Essa, A. A. (2013). β-Thalassemia in Abu Dhabi: consanguinity and tribal stratification are major factors explaining the high prevalence of the disease. Hemoglobin, 37(4), 351-358.
Origa, R.(2021). Genetic basis, pathophysiology and diagnosis of thalassaemias. In Cappellini, M.D., Farmakis, D., Poter, J., and Taher, A. (Eds.), Guidelines for the management of transfusion dependent thalassemia (TDT), (4th ed), Thalassemia international federation, pages 20-36.
Lee, J. S., Im Cho, S., Park, S. S., & Seong, M. W. (2021). Molecular basis and diagnosis of thalassemia. Blood Research, 56(S1), 39-43.
Kwiatkowski, J.L.(2016).Hemoglobinopathies, Thalassemias.In Lanzkowsky, P., Lipton, J., & Fish, J. D. (2016). Lanzkowsky's manual of pediatric hematology and oncology,(6th ed), Elsevier, pages 186-195.
Ehsan H, Wahab A, Anwer F, et al. (August 27, 2020) Prevalence of Transfusion Transmissible Infections in Beta-Thalassemia Major Patients in Pakistan: A Systematic Review. Cureus 12(8).
Bunn, H, F. and Sankaran, V.G.(2017). PART I Anemia and Red Cell Disorders,8- Thalassemia. In Aster, J.C.and Bunn, H.F.(Eds.), Pathophysiology of Blood Disorders,(2nd ed) McGraw-Hill, open I touch.
Zorina-Lichtenwalter, K., Lichtenwalter, R. N., Zaykin, D. V., Parisien, M., Gravel, S., Bortsov, A., & Diatchenko, L. (2019). A study in scarlet: MC1R as the main predictor of red hair and exemplar of the flip-flop effect. Human molecular genetics, 28(12), 2093-2106.
Nasti, T. H., & Timares, L. (2015). MC 1R, Eumelanin and Pheomelanin: Their role in determining the susceptibility to skin cancer. Photochemistry and photobiology, 91(1), 188-200.
Kaňková, Š., Bičíková, M., Máčová, L., Hlaváčová, J., Sýkorová, K., Jandová, D., & Flegr, J. (2021). Latent toxoplasmosis and vitamin D concentration in humans: three observational studies. Folia Parasitologica, 68, 1-7.
Molazem Z, Noormohammadi R, Dokouhaki R, Zakerinia M, Bagheri Z. The Effects of Nutrition, Exercise, and a Praying Program on Reducing Iron Overload in Patients With Beta-Thalassemia Major: A Randomized Clinical Trial. Iran J Pediatr. 2016;26(5):e3869. doi: 10.5812/ijp.3869.
Ozdemir, Z. C., Koc, A., Aycicek, A., & Kocyigit, A. (2014). N-Acetylcysteine supplementation reduces oxidative stress and DNA damage in children with β-thalassemia. Hemoglobin, 38(5), 359–364. https://doi.org/10.3109/03630269.2014.951890
Haghpanah, S., Cohan, N., Bordbar, M., Bazrafshan, A., Karimi, M., Zareifar, S., Safaei, S., Aramesh, A., Moghadam, M., Fard, S., & Zekavat, O. R. (2021). Effects of three months of treatment with vitamin E and N-acetyl cysteine on the oxidative balance in patients with transfusion-dependent β-thalassemia. Annals of hematology, 100(3), 635–644. https://doi.org/10.1007/s00277-020-04346-2
El-Haggar, S. M., El-Shanshory, M. R., El-shafey, R. A., & Dabour, M. S. (2018). Decreasing cardiac iron overload with Amlodipine and Spirulina in children with β-thalassemia. Pediatric hematology oncology journal, 3(3), 64-69.
Hussien, J., Al-Katib, S., & Al-Zuhairy, S. (2021). Role of Vitamin C Supplementation on Iron Overload and Oxidative Stress in Beta Thalassemia Major Patients in Maysan Province-Iraq. Kufa Medical Journal, 17(1), 111–127. https://doi.org/10.36330/kmj.v17i1.1954
Soeizi, E., Rafraf, M., Asghari-Jafarabadi, M., Ghaffari, A., Rezamand, A., & Doostan, F. (2016). Effects of Green Tea on Serum Iron Parameters and Antioxidant Status in Patients with β–Thalassemia Major. Pharmaceutical Sciences, 23(1), 27-36.
Koonyosying, P., Tantiworawit, A., Hantrakool, S., Utama-Ang, N., Cresswell, M., Fucharoen, S., ... & Srichairatanakool, S. (2020). Consumption of a green tea extract–curcumin drink decreases blood urea nitrogen and redox iron in β-thalassemia patients. Food & function, 11(1), 932-943.
Abotaleb, M., Samuel, S., Varghese, E., Varghese, S., Kubatka, P., Liskova, A., et al. (2018). Flavonoids in cancer and apoptosis. Cancers 11:28. doi: 10.3390/cancers11010028.